Project DUMBO
Collaborators
Norrlands University Hospital
Karolinska Hospital
Akademiska Hospital
Expertise
Design Research
Service Design
Sector
Healthcare
Date
January 2012 - June 2015
Challenge
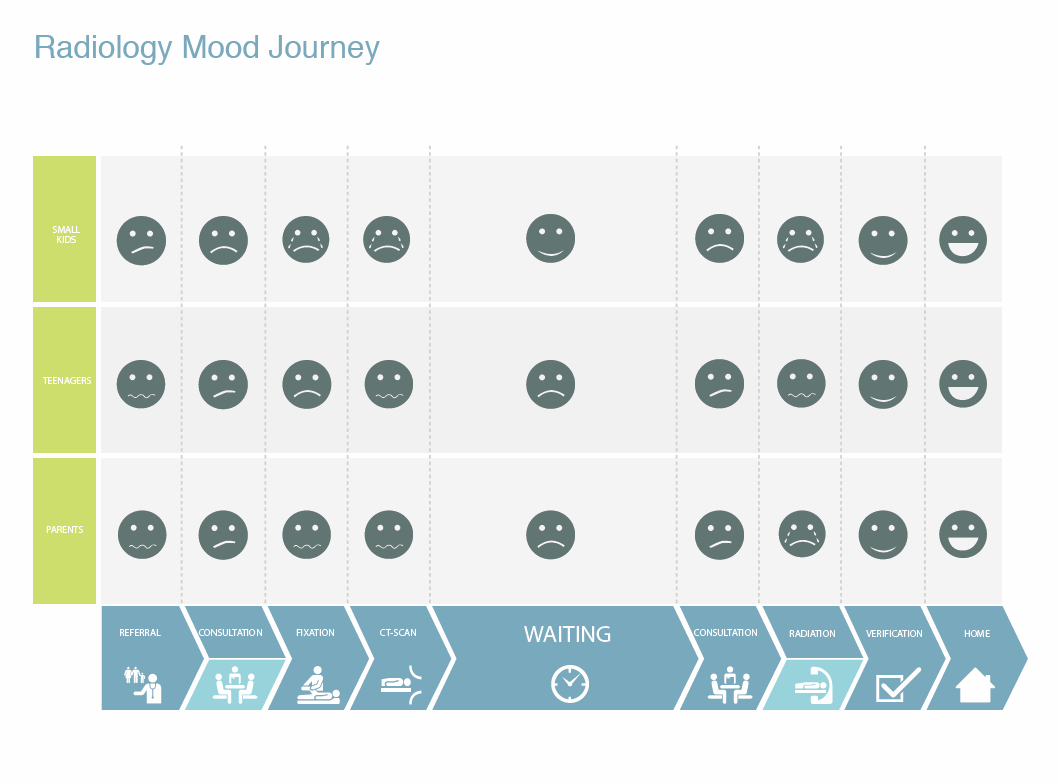
Young children undergoing radiotherapy often have to be sedated or anesthetized for their treatments because the process can be both stressful and challenging; the highly technological environment can be scary, the child must be left alone in the treatment room, and the child must lie completely still during the treatment.
General anesthesia can pose medical risks for the child. It can increase the side effects experienced by the children, and it can be very disruptive to their daily life routines, especially in regards to sleep and nutrition. It is also a very time consuming and costly procedure for radiotherapy departments, requiring the presence of specialist staff for each of the child’s radiotherapy treatments, which can last several weeks.
“We set out to create tools that could help reduce anxiety and fear levels in pediatric patients undergoing radiotherapy, thereby decreasing the usage of anesthesia and sedation during treatment sessions.”
Role
I was the lead design researcher on the project, and it was my responsibility to facilitate the research and development of a design intervention which we would test within our partnering hospitals.
- I organized and led a team of 12 design students in a 10-week Service Design course, where they conducted fieldwork, synthesized research findings into key insights, worked with radiotherapy experts to develop design directions, and generated a series of service concepts.
- I organized and ran an 11-week Summer Design studio with two student interns, where we worked together to transform the service design concepts into a final cohesive design.
- I was responsible for the implementation of the design intervention within the radiotherapy departments at the participating hospitals.
- I coordinated the collaboration between UID and the project’s many stakeholders.
Process
PHASE 1: Service Design Course
Ethnographic Fieldwork
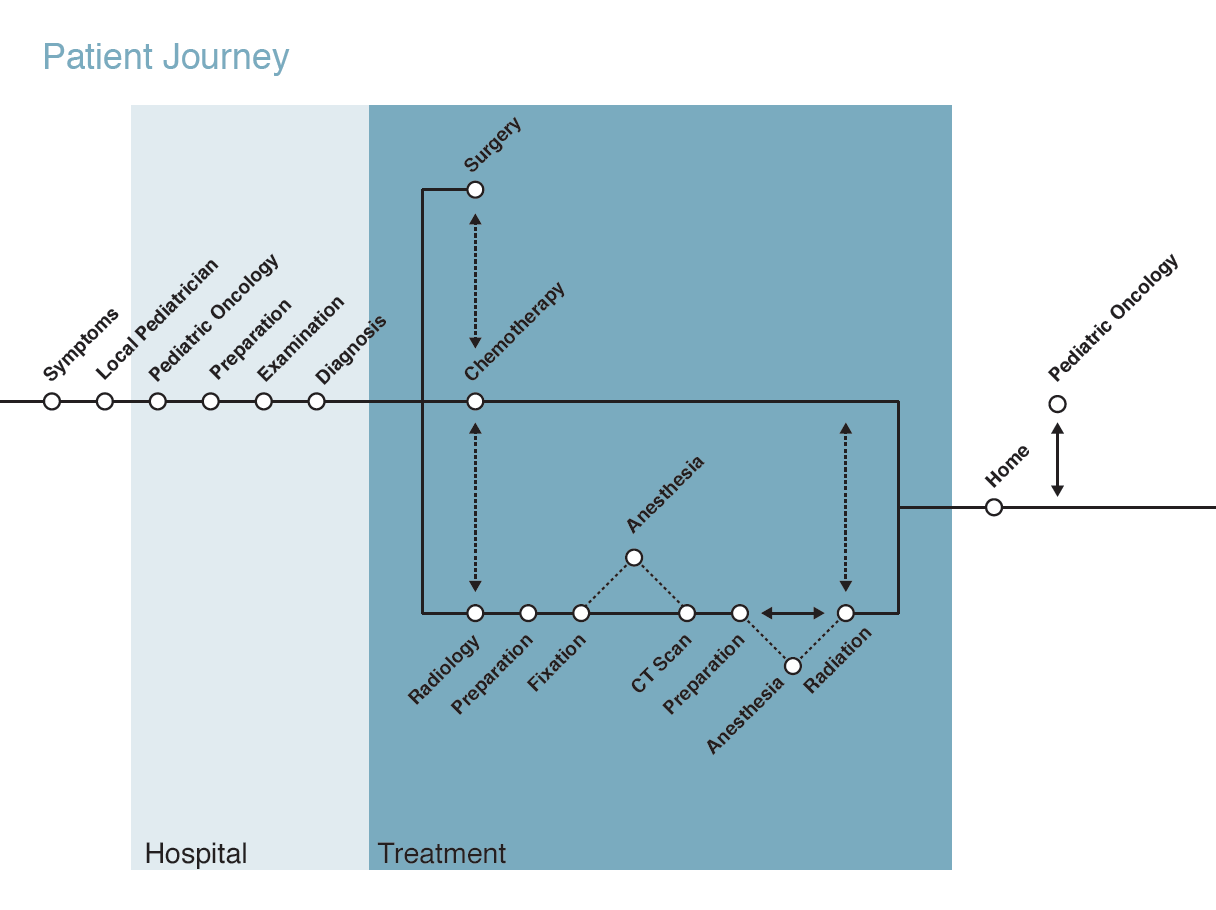
My team conducted short field investigations at each participating hospital, in both the radiotherapy departments as well as the pediatric oncology wards.
Interviews with care providers, patients and their families
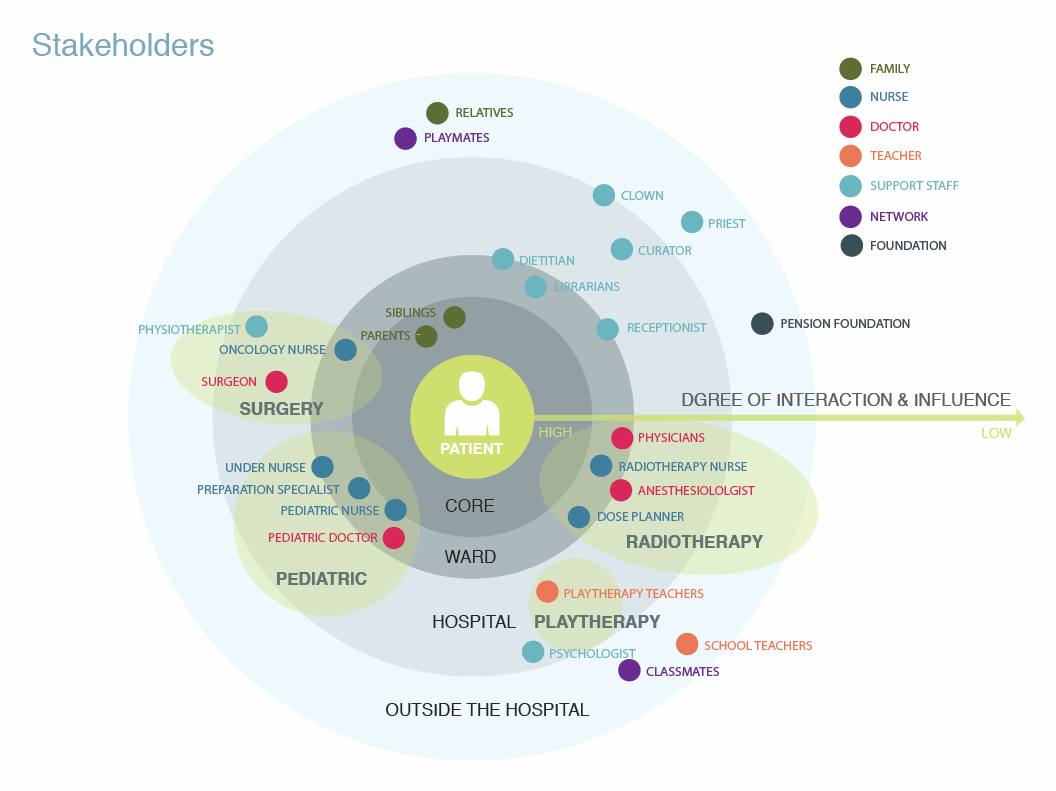
My team conducted interviews with a wide variety of individuals involved in the pediatric radiotherapy care chain: oncology doctors and nurses, radiotherapy nurses, and play therapists. They also drew on interviews of over 16 children and their parents talking about their radiotherapy experiences, conducted by the nursing researchers involved in the project.
Synthesis
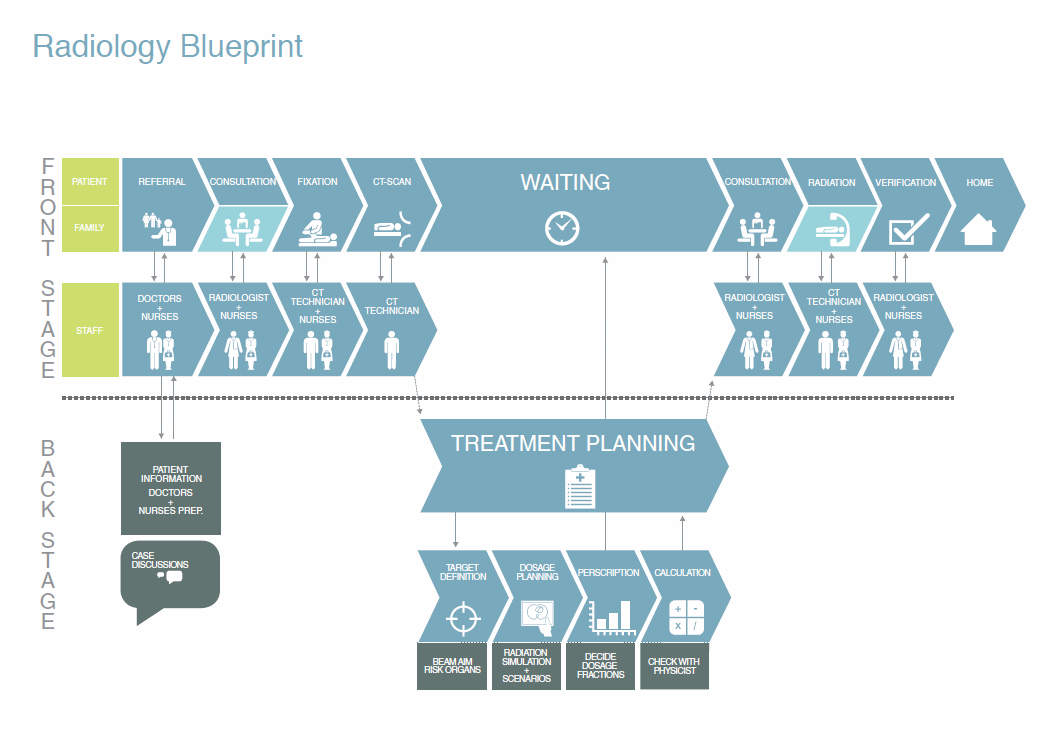
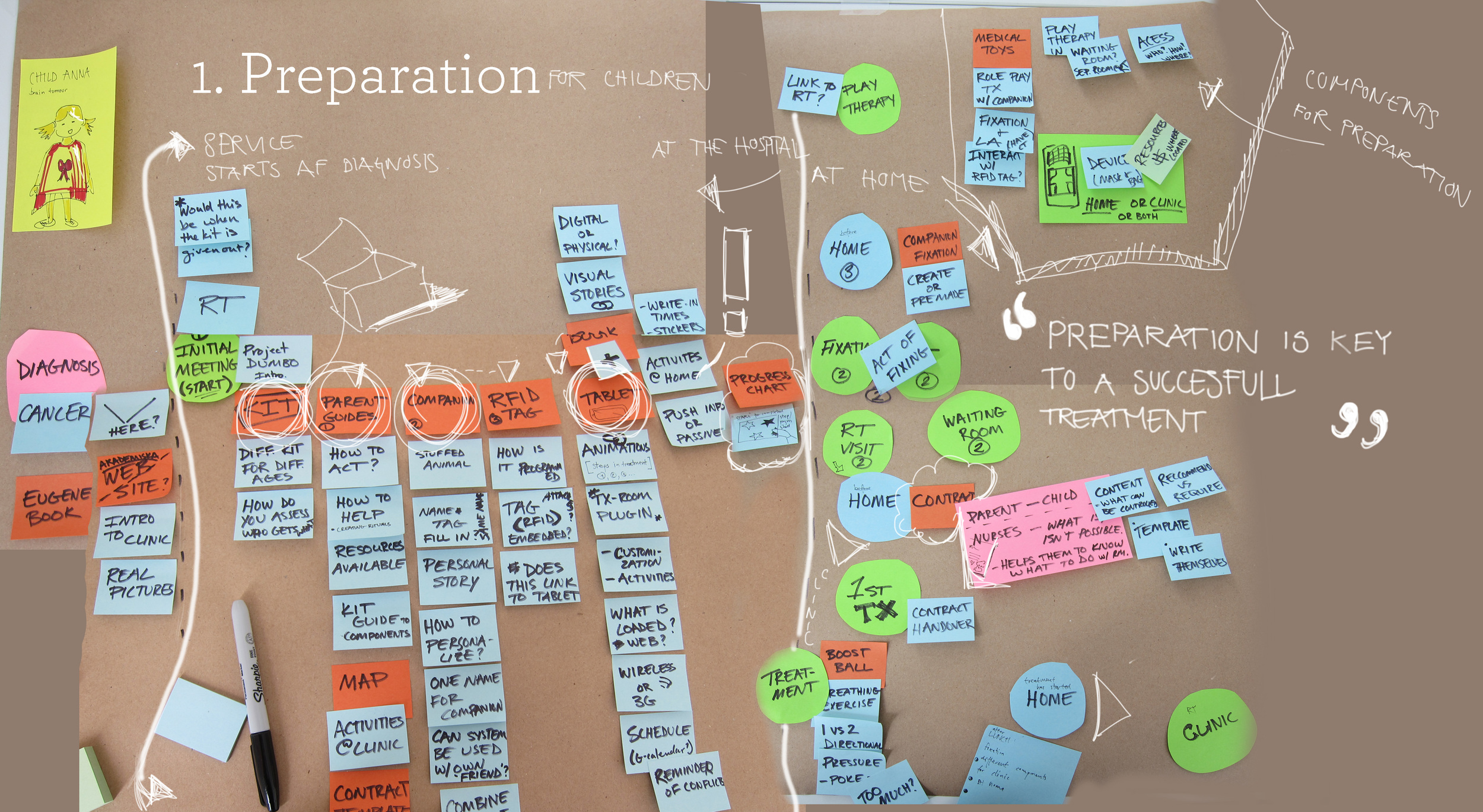
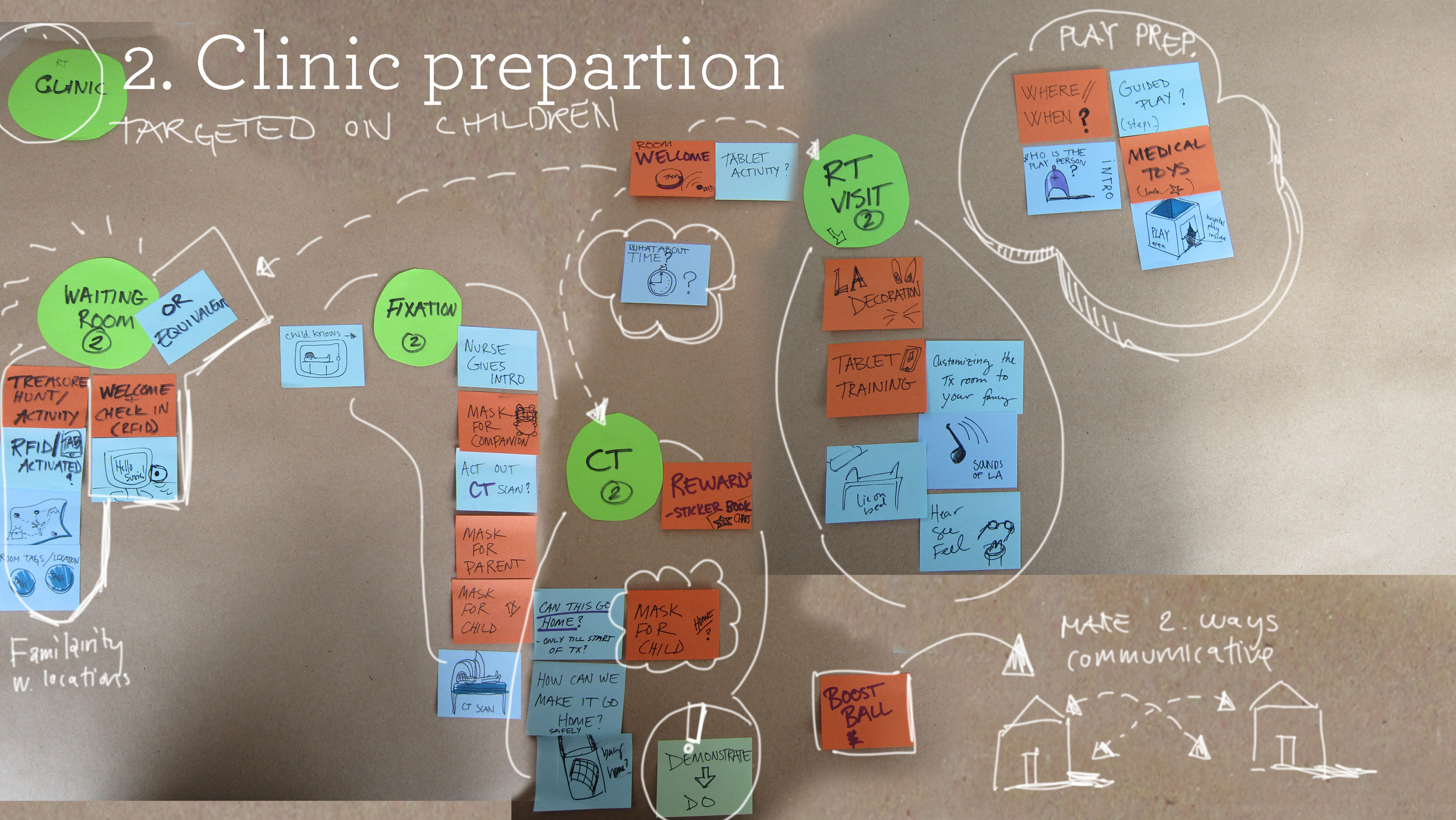
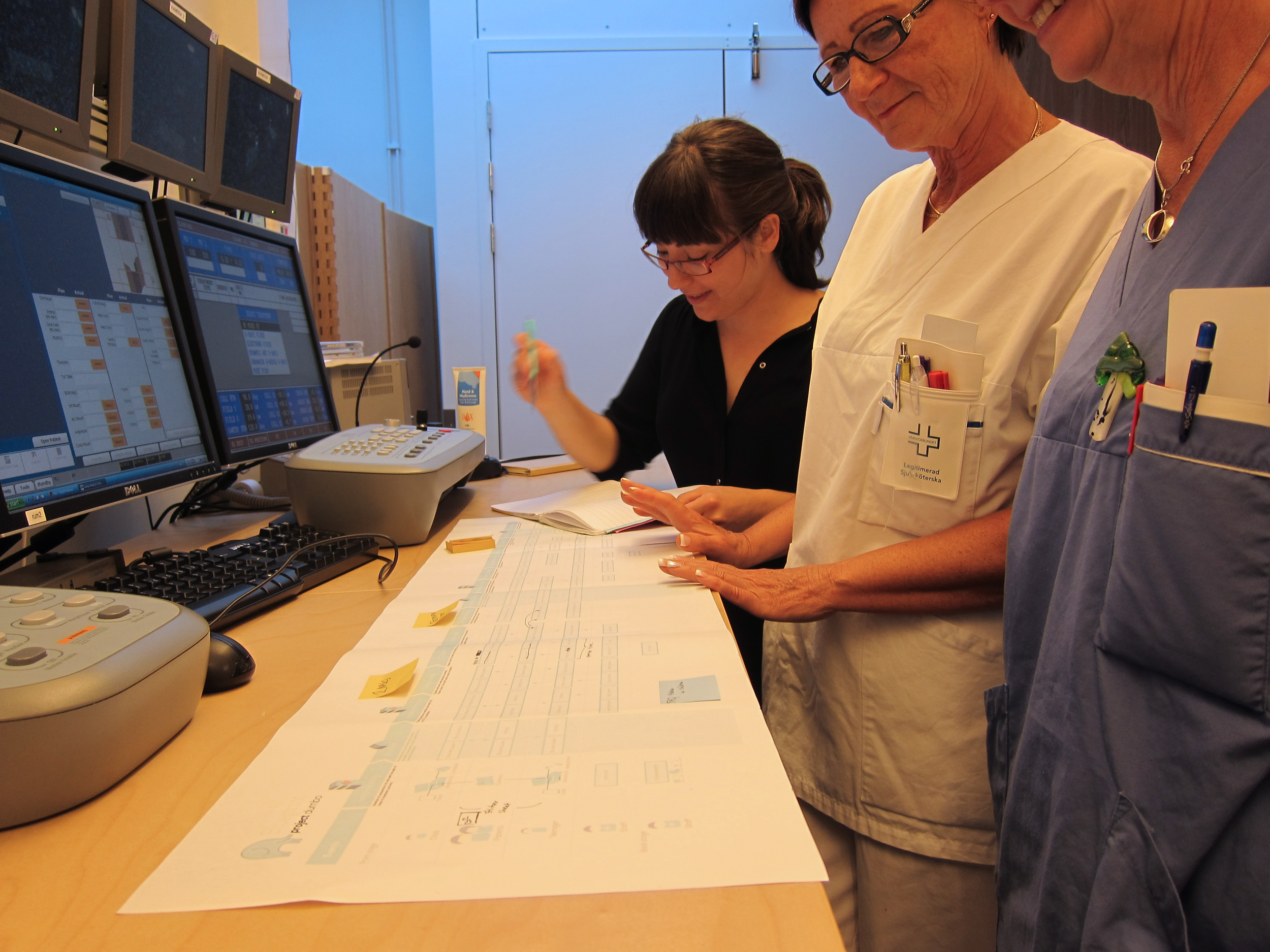
My team used a variety of service design methods to visually analyze the material gathered through their research: journey maps, blueprints, stakeholder maps, and emotional experience maps. They also identified key findings from across the consolidated research material for all three hospitals.
Insights
- There is a lack of appropriate information for children and parents about radiotherapy and what to expect.
- The radiotherapy experience is tailored towards adults because there are much higher numbers of adults being treated than children.
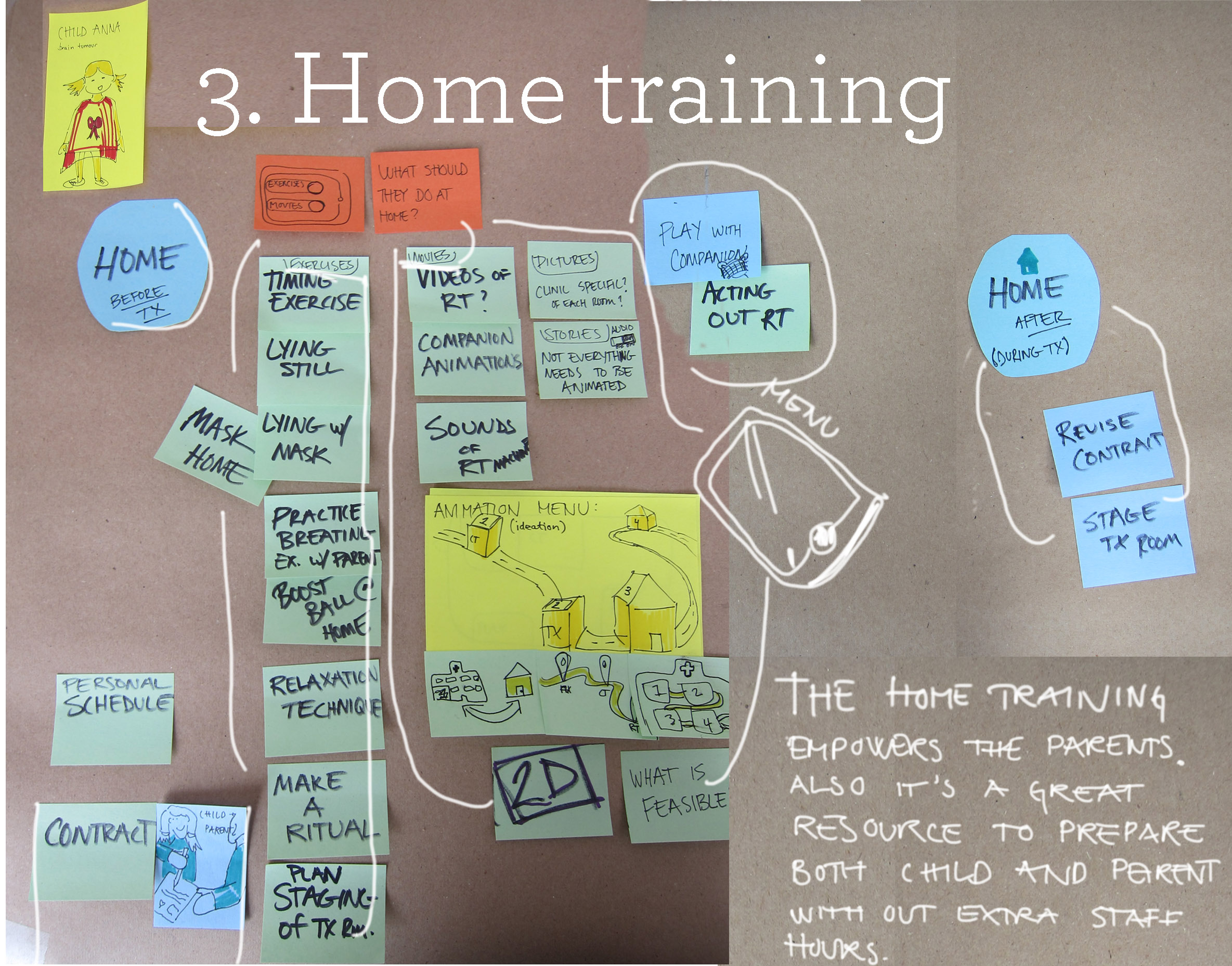
- Information is primarily given at the clinic. There is a lack of preparation materials that can be utilized in the home environment. This would also enable the parents to become more involved in the process.
Ideation with Stakeholders
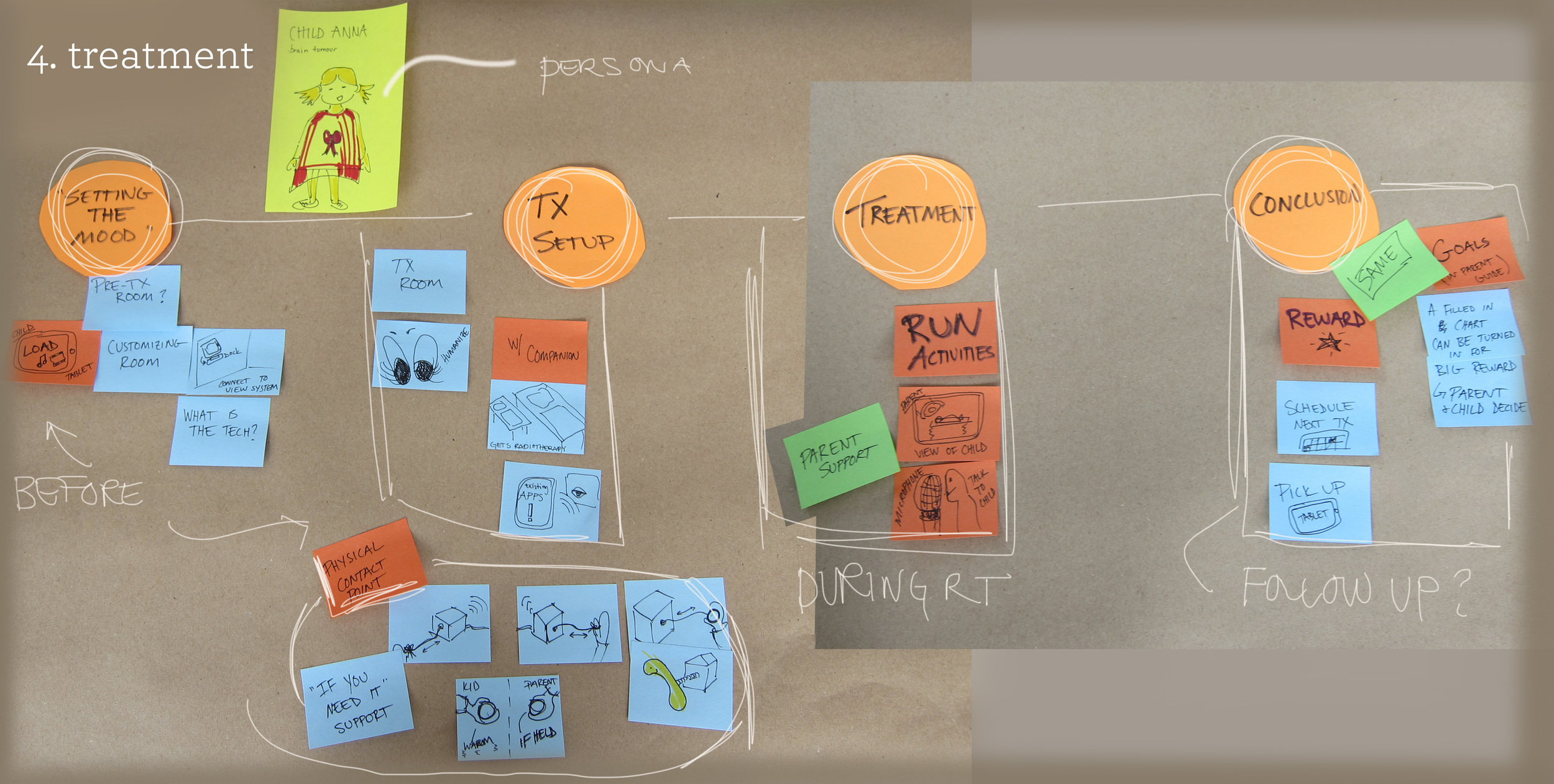
I broke the group down into four smaller teams after the research phase. Each team conducted workshops with the doctors and nurses involved in the project, to ideate and refine possible design directions.
Concept Development
Each team worked to develop a service design concept that would address the needs of children going through radiotherapy, both before and during treatment.
PHASE 2: Summer Design Studio
Design Refinement
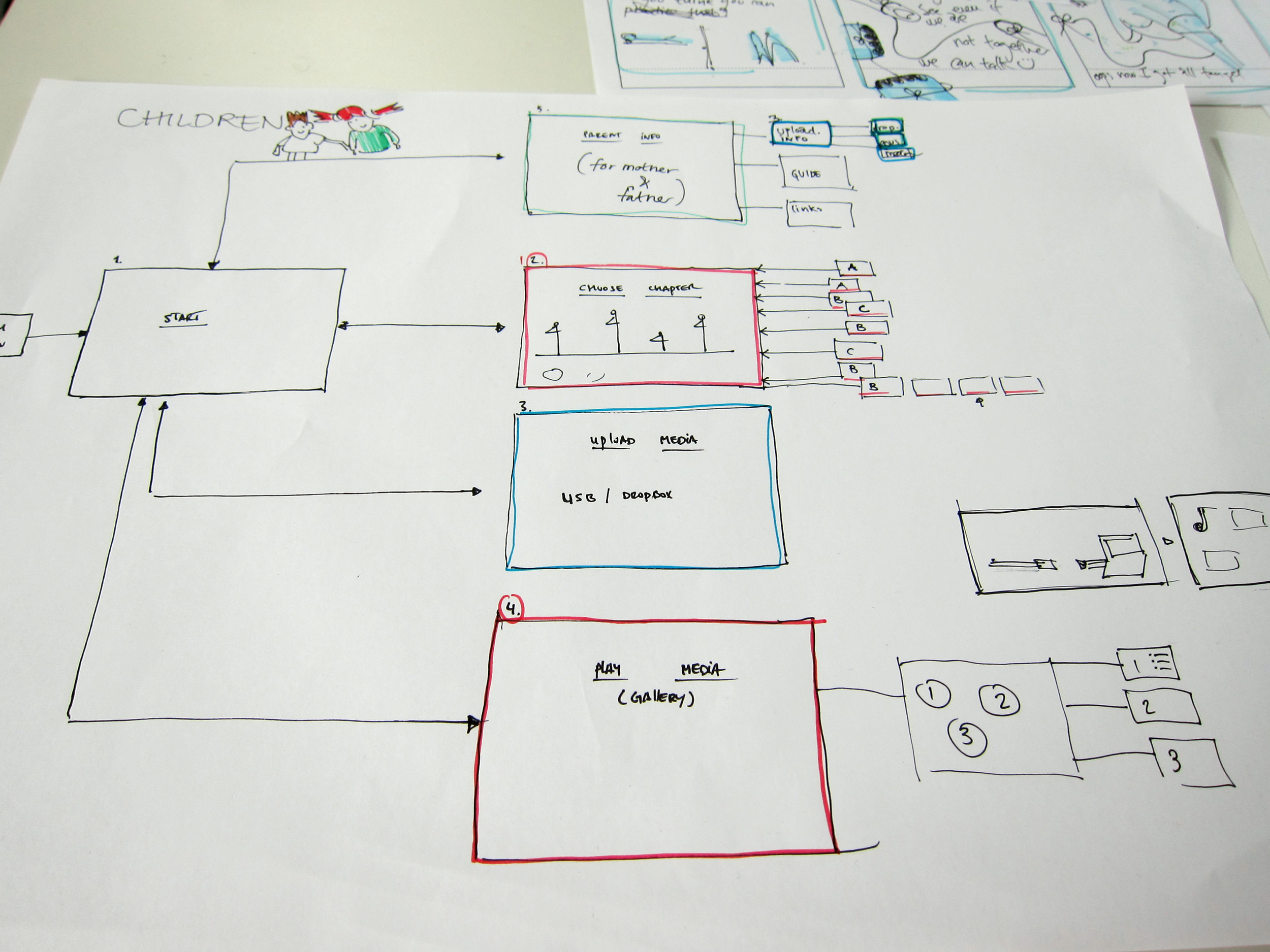
We met with the doctors and nurses involved in the project to assess the feasibility of the design concepts. Working with their feedback, we brainstormed ideas and consolidated the strengths of the different concepts into a new design concept. We blueprinted the service and its touchpoints, and met with radiotherapy nurses to reassess the feasibility of the new concept.
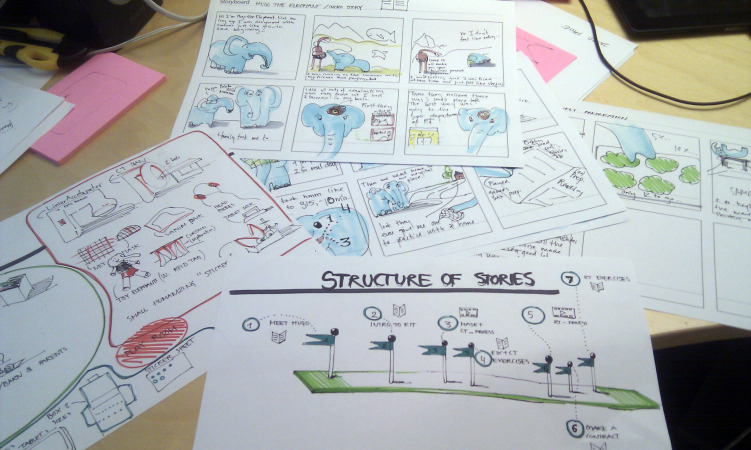
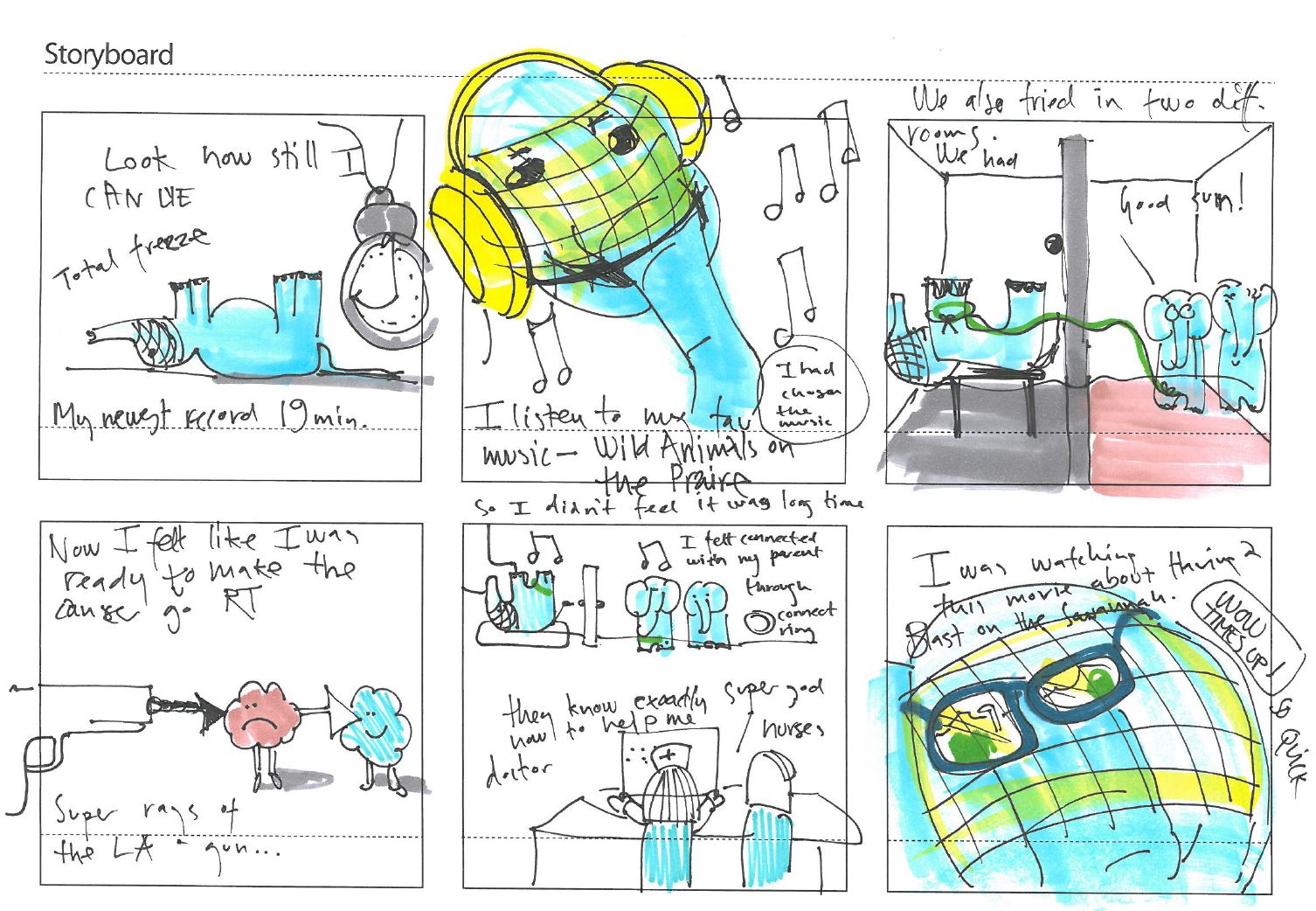
Storytelling
Because our concept was centered on a character who would guide the child through the radiotherapy process, we spent a lot of time developing the stories which would support this character.
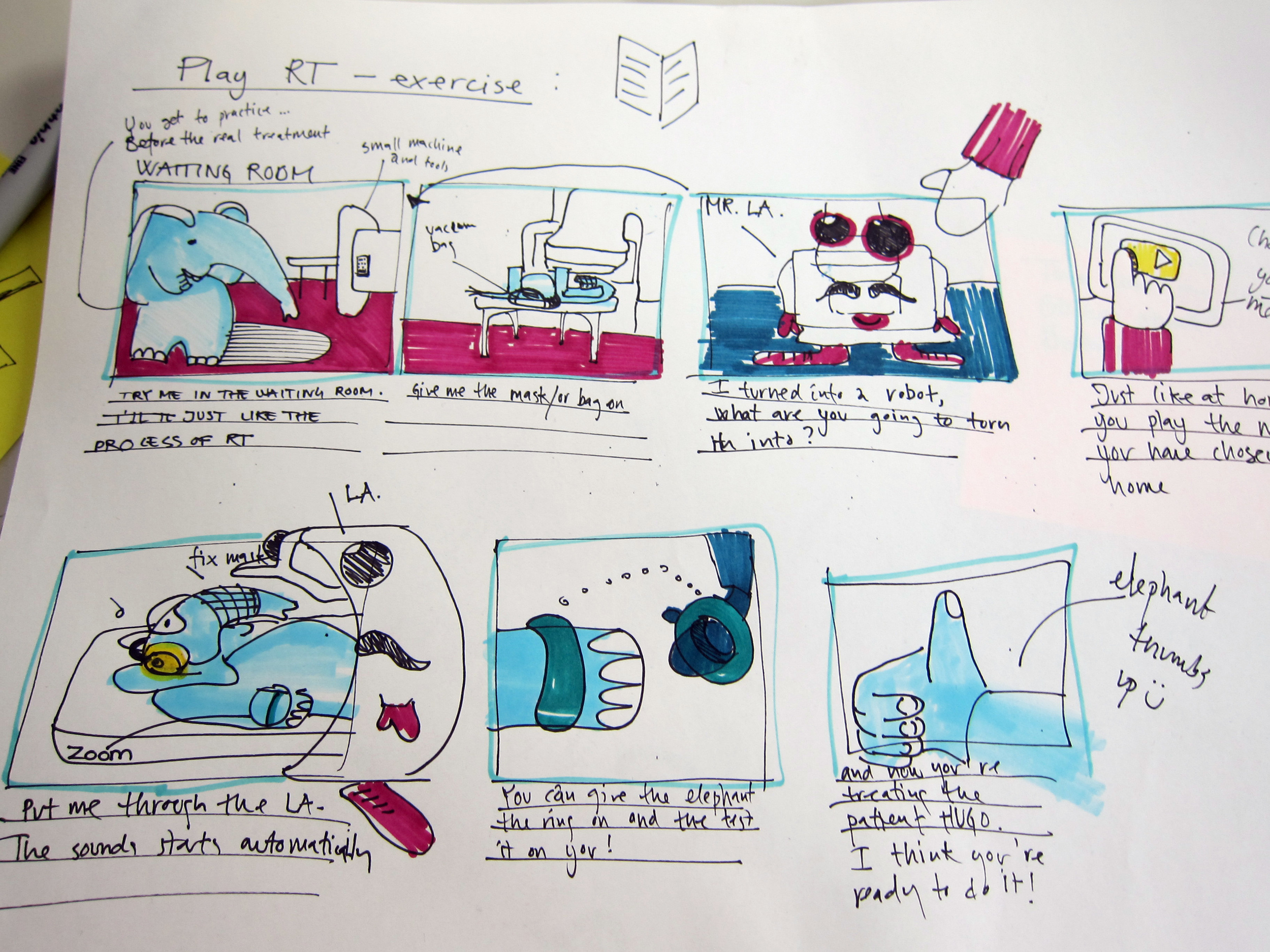
Physical and Digital Prototyping
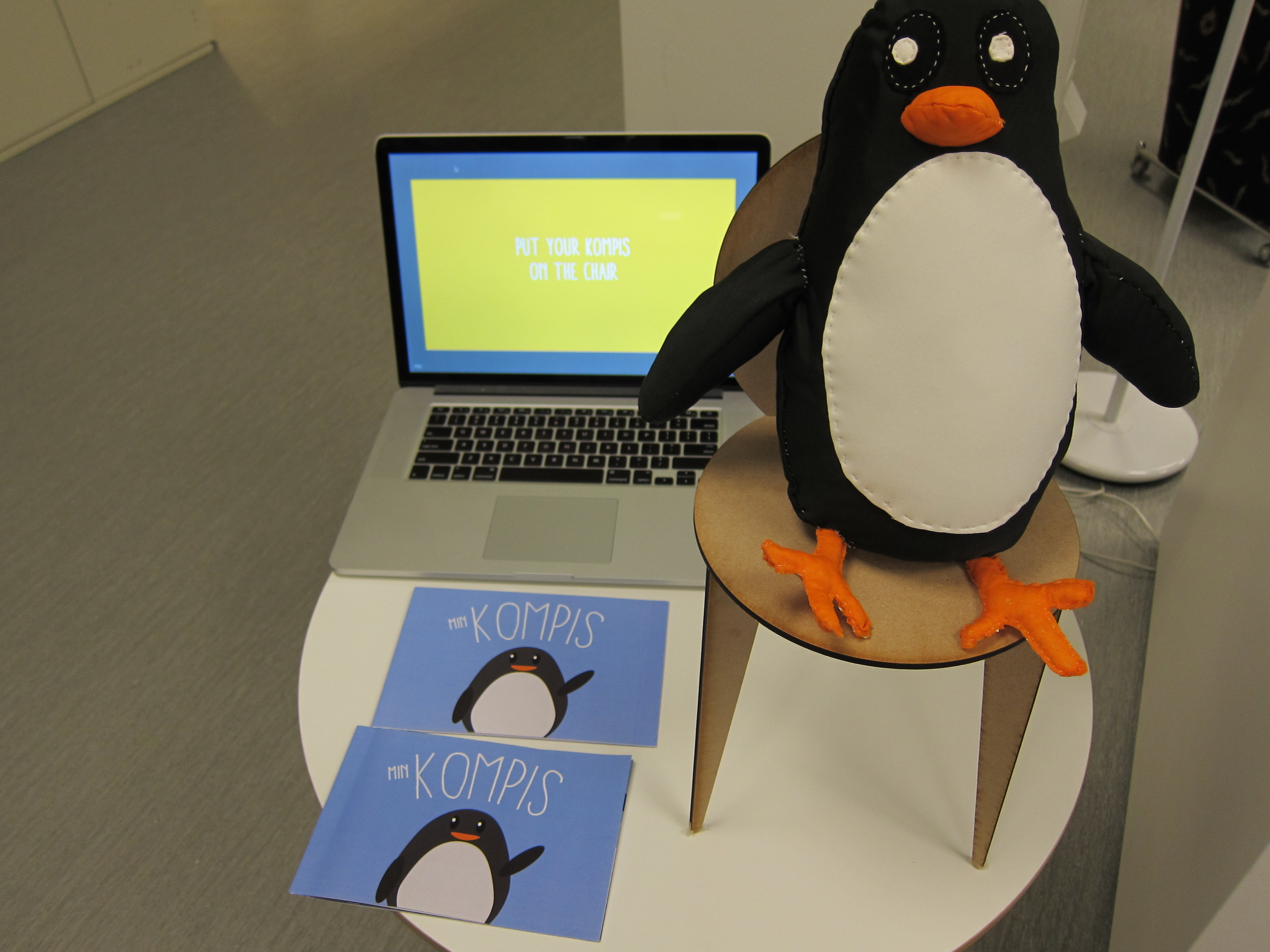
Because our service concept involved both physical and digital components, we built a wide variety of prototypes to test out different aspects of the concept, such as: wireframes, app sketches, paper mockups, and foamcore models.
User Testing
We tested all of our materials with both children and the radiotherapy staff from the hospitals, to ensure the usability and accuracy of the materials.
Result
HUGO for Kids
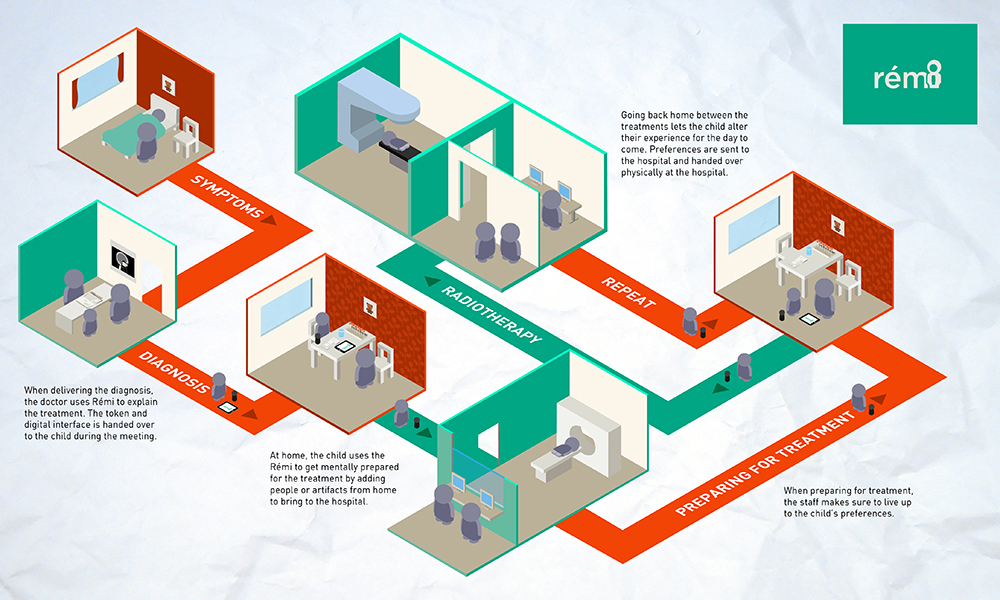
HUGO is a service that is focused on providing a cohesive care experience for children with cancer and their parents, from time of diagnosis to the end of treatment, which focuses on providing tools to inform, prepare, and engage the child through the radiotherapy journey.
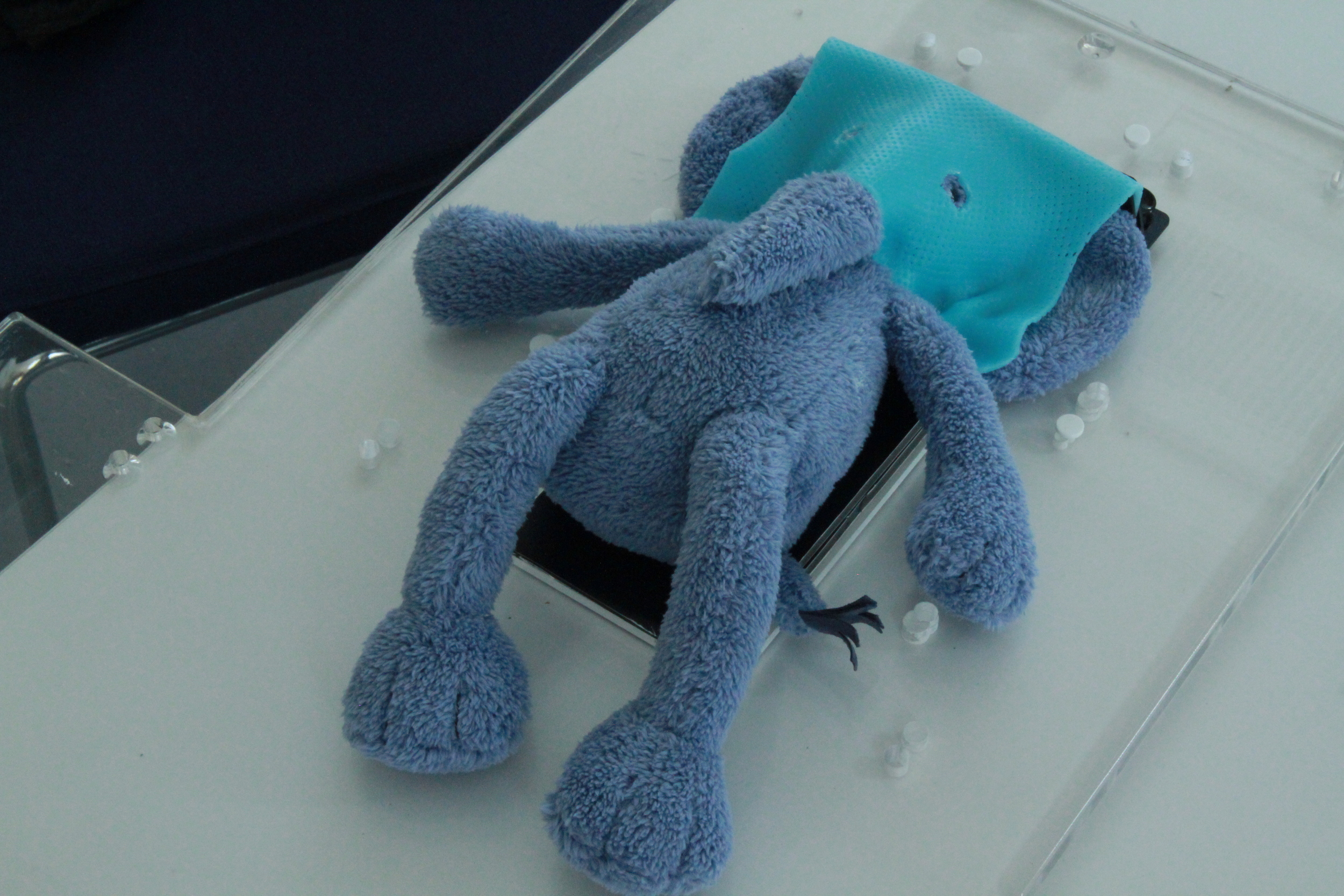
HUGO consists of a preparatory kit that is designed to be distributed to children before they start their radiotherapy treatment, which provides age appropriate information about radiotherapy treatment and what to expect. The kit contains an android tablet installed with the HUGO application, a Parent Booklet which provided important information to the parents, and a gift of a stuffed elephant for the child.
The HUGO application contains stories, animations and exercises for the child to do at home with their parents to help them understand and prepare for their radiotherapy treatments. All of these stories involve our main character, Hugo the elephant, who has experience with radiotherapy treatment when he had a lump in his head. Hugo acts as a guide for the child, both within the App, but also in physical form, represented by the stuffed elephant provided in the kit.
The kit is provided to the child at their radiotherapy treatment consultation appointment, so they can take it home with them to prepare for treatment. There are also play therapy toys available at the Radiotherapy Clinic designed for the child to play out their radiotherapy experiences with toys in a safe and supportive environment. These toys are interactive small-scale versions of the computed-tomography (CT) and radiotherapy (RT) machines, as well as small vacuum bag and face mask fixation devices that can be used on stuffed animals and dolls.
The tablet can also be used in combination with video goggles within the treatment room, so that the child can watch movies or listen to their favorite music while they are receiving radiation.
Impact
HUGO was implemented within our three collaborating hospitals for 1.5 years and assessed for its impact upon child and parent anxiety levels during radiotherapy. The feedback from the DUMBO team suggests that the HUGO for Kids intervention was successful in informing both the child and their parents about radiotherapy, and allowed a way for the parents to be more involved in their child’s care process and not as dependent upon the care staff in preparing their child for treatment.
While the HUGO for Kids intervention was specifically designed for young children going through radiotherapy and their parents, through use, the material reached beyond these actors to other individuals also involved in the child’s life, such as siblings and friends